
Rabies is a deadly virus spread to people from the saliva of infected animals. The rabies virus is usually transmitted through a bite. Animals most likely to transmit rabies in the United States include bats, coyotes, foxes, raccoons and skunks. Rabies is a fatal viral disease caused by a Lyssavirus.
Rabies is caused by a virus belonging to the genus Lyssavirus in the family Rhabdoviridae.
Cause of Rabies:
- Agent: Rabies virus (Rabies lyssavirus).
- Type: RNA virus with a characteristic bullet-shaped structure.
- Variants: Different Lyssavirus species can cause rabies-like disease, but Rabies lyssavirus is the main cause worldwide.
- Hosts: All warm-blooded mammals (domestic and wild) can be infected and act as reservoirs.
Rabies is caused by the rabies virus, a deadly neurotropic virus that targets the nervous system

Key facts
- Rabies is a serious public health problem in over 150 countries and territories, mainly in Asia and Africa. It is a viral, zoonotic, neglected tropical disease that causes tens of thousands of deaths annually, with 40% being children under 15.
- Dog bites and scratches cause 99% of the human rabies cases, and can be prevented through dog vaccination and bite prevention.
- Once the virus infects the central nervous system and clinical symptoms appear, rabies is fatal in 100% of cases.
- However, rabies deaths are preventable with prompt post exposure prophylaxis (PEP) by stopping the virus from reaching the central nervous system. PEP consists of thorough wound washing, administration of a course of human rabies vaccine and, when indicated, rabies immunoglobulins (RIG).
- If a person is bitten or scratched by a potentially rabid animal, they should immediately and always seek PEP care.
- WHO and its global partners aim to end human deaths from dog-mediated rabies through a comprehensive One Health approach promoting mass dog vaccination, ensuring access to PEP, health worker training, improved surveillance, and bite prevention through community awareness.
Overview
Dog-mediated rabies
Rabies is a vaccine-preventable, zoonotic, viral disease affecting the central nervous system. In up to 99% of the human rabies cases, dogs are responsible for virus transmission. Children between the age of 5 and 14 years are frequent victims.

Rabies infects mammals, including dogs, cats, livestock and wildlife.
Rabies spreads to people and animals via saliva, usually through bites scratches, or direct contact with mucosa (e.g. eyes, mouth, or open wounds). Once clinical symptoms appear, rabies is virtually 100% fatal.
The global cost of rabies is estimated to be around US$ 8.6 billion per year including lost lives and livelihoods, medical care and associated costs, as well as uncalculated psychological trauma.
Rabies is present on all continents except Antarctica. Globally there are an estimated 59 000 deaths from rabies annually; however, due to underreporting, documented case numbers often differ from the estimate.
- Cause: Rabies is a fatal viral disease caused by a Lyssavirus.
- Transmission: Spread mainly through the bite or saliva of an infected animal.
- Affected animals: All warm-blooded mammals can get rabies (dogs, cats, cattle, horses, wildlife like bats, foxes, raccoons).
- Signs: Behavior changes (aggression, restlessness, paralysis, excessive salivation, difficulty swallowing), followed by progressive neurological signs and death.
- Course: Once clinical signs appear, the disease is almost always fatal.
- Prevention: Vaccination of pets, livestock, and at-risk wildlife; controlling stray dog populations; avoiding contact with wild animals.
- Public health importance: Zoonotic – rabies can be transmitted to humans, making it a major public health concern.
How Rabies spread:
Rabies spreads mainly through direct contact with infected saliva or nervous tissue. Here are the key routes:
- Bites: The most common way. The virus enters through the wound when an infected animal bites another animal or a human.
- Scratches / open wounds: If saliva from a rabid animal contaminates fresh cuts, abrasions, or mucous membranes (eyes, mouth, nose).
- Organ or tissue exposure (rare): In humans, very rarely from corneal or organ transplants.
- Not spread by: Blood, urine, feces, or casual contact (like petting a rabid animal without open wounds).
⚠️ Important: Once the virus enters, it travels along the nerves to the brain, multiplies, and then spreads to the salivary glands, ready to infect another host.
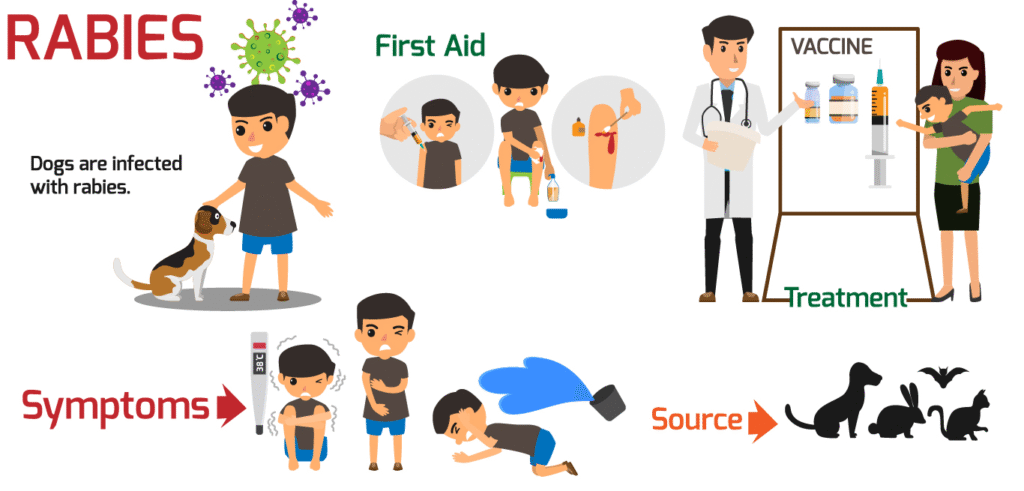
Treatment
No, as such treatment because it is viral disease, recommend only vaccination for that.
Rabies treatment depends on whether exposure has happened or clinical signs have already developed:
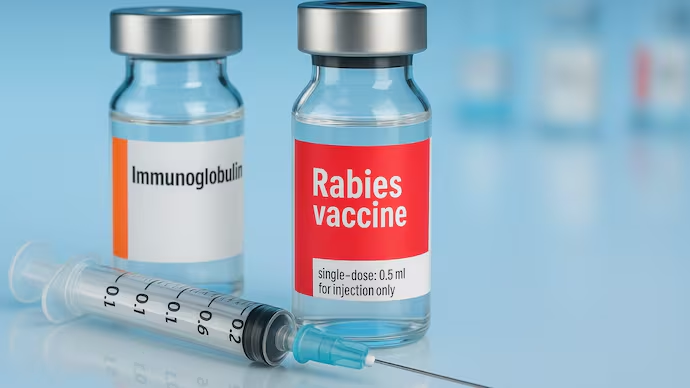
After Exposure (Before Symptoms Appear) → Post-Exposure Prophylaxis (PEP)
- Immediate wound care: Wash the bite/scratch thoroughly with soap and running water for at least 15 minutes. Apply antiseptic (iodine, alcohol).
- Rabies vaccine: Series of injections to train the immune system to fight the virus.
- Rabies immunoglobulin (RIG): Given in severe exposures (Category III bites) to provide instant antibodies, infiltrated around the wound and the rest intramuscularly.
- Tetanus prevention & antibiotics: May also be required for bite wounds.
PEP is highly effective if started promptly, before symptoms develop.
After Clinical Signs Appear
- Unfortunately, there is no effective treatment once rabies symptoms start.
- The disease is almost always fatal in both animals and humans.
- Supportive/palliative care may be provided, but survival is extremely rare.
Best strategy: Prevention through vaccination of animals and humans at risk, plus immediate post-exposure care.
Rabies prevention and control
in animals focus mainly on regular vaccination of pets and livestock, mass dog vaccination campaigns, and controlling stray dog populations to stop the spread of the virus. In some regions, oral rabies vaccines are used in wildlife such as foxes and raccoons. Good responsible pet ownership and reporting of suspected cases are also essential to reduce transmission.
Summary
Rabies is a fatal viral disease caused by the Rabies lyssavirus, which affects all warm-blooded mammals, including humans. It is primarily spread through the bite or saliva of an infected animal, most often dogs, bats, and wild carnivores. After entering the body, the virus travels along the nerves to the brain, causing neurological signs such as aggression, paralysis, excessive salivation, and difficulty swallowing. Once clinical signs appear, rabies is almost always fatal, and there is no effective treatment. However, the disease can be prevented through immediate wound washing, post-exposure prophylaxis (rabies vaccine and immunoglobulin), and routine vaccination of pets and livestock. Prevention and control through vaccination and avoiding contact with suspected rabid animals remain the most effective ways to protect both animals and humans.
FAQs about Rabies
1. What is rabies?
Rabies is a deadly virus that attacks the brain and nerves of mammals, including humans.
2. How do people get rabies?
Mostly through bites or scratches from infected animals, or contact with their saliva.
3. Which animals spread rabies the most?
Dogs are the main source worldwide, but bats, foxes, raccoons, and skunks can also carry it.
4. Can rabies be prevented?
Yes—by vaccinating pets, avoiding wild animals, and getting medical help (PEP) after possible exposure.
5. Is rabies curable?
No. Once symptoms appear, it is almost always fatal. Prevention is the only protection.
Email Us
Have a question, suggestion, or collaboration request?
Send us an email at:
Need Veterinary Help?
If you have any questions about animal health, management, diseases, or treatment, feel free to reach out. Our professional veterinary team is available to assist you.






https://shorturl.fm/KkWcg